2D Dental Radiography Interpretation Online Course
Advance your radiographic interpretation skills with Dr. Sholapurkar's in-depth course, tackling dental pathologies and refining diagnostic acumen through interactive case discussions.
8 Chapters
5 hrs
5 CE/CPD
Systematic approach to interpretation of extraoral and intraoral radiographs
Dive deeper into dental radiographic interpretation with Dr. Amar Sholapurkar's 2D Radiography Interpretation course. Building upon the foundational skills, this engaging session delves into dental cases, differential diagnoses, and considerations.
Through the recordings of the interactive discussions and a wealth of clinical images, Dr. Sholapurkar helps participants in refining their diagnostic acumen for pathologies commonly encountered in dental practice.
Suitable for general dentists, this course empowers clinicians to elevate their radiographic interpretation skills and enhance patient care under the instruction of an experienced oral radiology educator.
Course Outline
What will I learn by taking this course?
Sample the Online Course Content Below!
Get unlimited access to 5 hours of 2D Radiography training, complete with many tips and tricks from an experienced Dental Radiology educator.
With lifetime access, you can revisit the course whenever you need at your own pace.
All course lessons are available with English subtitles.
Here’s what’s included:
8 Chapters - 17 Video Lessons
CPD/CE Hours: 5
01 - 01 - Introduction and Overview of Course
- Recognize normal anatomic landmarks on radiographs, providing a solid foundation for identifying abnormalities.
- Systematically analyze clinical pictures and radiographs, simulating real-world patient scenarios to enhance diagnostic abilities.
- Differentiate between normal entities and pathologies, ensuring accurate diagnoses and appropriate treatment planning.
- Confidently arrive at diagnoses independently, empowering you to make informed decisions in your dental practice.
- Engaging in interactive discussions and workshops fosters a deeper understanding of radiographic interpretation.
- Apply the knowledge gained from analyzing over 300 clinical pictures and radiographs to real-world patient cases.
01 - 02 - Normal Dental Radiographic Landmarks and Variants
- Identify and describe various normal anatomic structures on radiographs, such as the incisive foramen, nasopalatine canal, and pterygomaxillary fissure.
- Recognize normal variants like the nasolacrimal canal, lateral fossa, and glossopharyngeal air space, preventing misdiagnosis as pathologies.
- Understand the importance of the pterygomaxillary fissure in diagnosing Le Fort fractures and maxillary sinus pathologies.
- Differentiate between normal periodontal ligament space variations and pathological widening, ensuring accurate assessment of periodontal health.
- Integrate radiographic findings with clinical examination and patient history to arrive at accurate diagnoses, emphasizing the role of radiographs as diagnostic aids.
01 - 03 - Differentiating Cervical Burnout from Dental Caries on 2D Radiographs
- Understand the radiographic appearance and etiology of cervical burnout, recognizing it as a normal radiographic finding rather than a pathology.
- Identify the key radiographic features that distinguish cervical burnout from dental caries, such as location, shape, and the presence or absence of enamel knife-edge destruction.
- Integrate radiographic findings with clinical examination techniques, such as probing, to confirm the presence or absence of dental caries.
- Appreciate the importance of taking multiple radiographs from different angles to avoid misdiagnosis and ensure accurate interpretation.
02 - 01 - A Systematic Approach to Dental Panoramic Radiograph Interpretation
- Understand the importance of knowing normal radiographic anatomy, variants, and common pathologies for accurate interpretation.
- Differentiate between normal anatomic structures and pathologies by assessing their characteristics, such as bilaterality, symmetry, and location.
- Identify and describe key normal anatomic landmarks on panoramic radiographs.
- Recognize and explain the concept of double real images in panoramic radiographs, which occur due to the projection of midline structures.
- Identify and differentiate various air spaces visible on panoramic radiographs, such as the glossopharyngeal, palatoglossal, and nasopharyngeal air spaces.
- Apply patient positioning techniques to minimize the appearance of undesirable air spaces, such as the palatoglossal air space, which can obscure important anatomic structures.
02 - 02 - A Case-Based Guide to Dental Panoramic Radiographs
Understand the importance of a comprehensive patient history and clinical examination in guiding radiographic interpretation.
- Apply a systematic and sequential method for interpreting panoramic radiographs, ensuring that all areas are thoroughly assessed and no pathologies are missed.
- Recognize the significance of evaluating both dental and non-dental structures in the panoramic radiograph, as the entire image is the responsibility of the dental professional.
- Identify multiple pathologies in a single radiograph by assessing the entire image rather than focusing solely on the area of interest.
- Appreciate the role of histopathological examination as the gold standard for definitive diagnosis, while recognizing the value of radiographic interpretation in providing differential diagnoses.
- Understand the importance of reviewing images in a relaxed state to minimize the risk of overlooking important findings.
03 - 01 - Decoding Dental Radiographic Lesions
- Determine whether a lesion is odontogenic or non-odontogenic based on its location relative to the inferior alveolar nerve canal or the maxillary antrum.
- Understand the significance of a lesion's site and location in narrowing down the differential diagnosis.
- Assess the size of a lesion using measuring tools and describe its dimensions in millimeters or centimeters.
- Analyze the shape of a lesion and understand how it relates to the likelihood of various pathologies, such as cysts, tumors, or abscesses.
- Evaluate the borders of a lesion and recognize how different border characteristics, such as corticated, sclerotic, or ill-defined borders, are associated with specific pathologies.
03 - 02 - Internal Structures and Surrounding Effects - Lesion Analysis
- Describe the internal structure of lesions using terms such as radiolucent, radiopaque, or mixed, and recognize how these characteristics relate to specific pathologies.
- Identify the presence of septae or calcifications within lesions and understand their diagnostic significance.
- Recognize the effects of lesions on surrounding structures, such as bone resorption or formation, and interpret these changes in the context of inflammatory diseases.
- Understand how space-occupying lesions create their own space by displacing adjacent structures, such as teeth, the maxillary sinus, or the inferior alveolar nerve canal.
- Identify root resorption and relate this finding to the presence of trauma, cysts, or slow-growing benign tumors.
- Recognize cortical bone expansion as a characteristic feature of benign, slow-growing tumors or cysts.
- Apply a systematic approach to radiographic interpretation using the "4S and IE" method, which includes assessing site, size, shape, surface (borders), internal structure, and effects on surrounding structures.



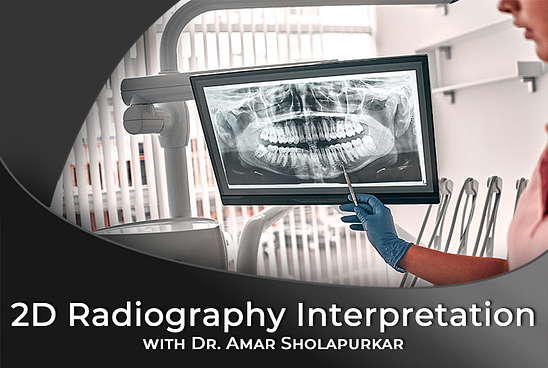
Unveiling the Secrets of Dental Radiography
Dive deeper into dental radiographic interpretation with Dr. Amar Sholapurkar's 2D Radiography Interpretation course.
Learn Different Features
Learn different radiographic features of maxillary sinus disorders, soft tissue calcifications, and more
Systematic Case Navigation
Navigate common cases through systematic, step-by-step radiographic analysis
Differentiate Similar Entities
Confidently differentiate between similar-appearing entities using key diagnostic criteria
Understand Clinical Implications
Understand the clinical implications and considerations for various radiographic findings
Interactive Knowledge Application
Engage in interactive case discussions to solidify knowledge application and critical thinking skills
Learn from an Experienced Educator
Learn from a seasoned oral radiology educator with extensive teaching experience
2D Dental Radiography interpretation
Online Course
$495 USD

You are Fully Protected by Our 100% Satisfaction-Guarantee.
I am confident that you will love this course, if you purchase the course and are not satisfied with the quality or content of the training, then let me know within 30 days of your purchase and I will refund you in full.
No questions asked.
Dr Ahmad Al-Hassiny
Founding Director of the Institute of Digital Dentistry
Meet Your Educator
Dr Amar Sholapurkar
BDS, MDS (Oral Medicine and Radiology)
Dr. Amar Sholapurkar is a highly accomplished academician and clinician with extensive global experience in dental radiology and education. Currently serving as discipline lead of Oral Radiology and Senior Lecturer (Clinical Dentistry and Oral Radiology) at the College of Medicine and Dentistry, James Cook University (JCU), Cairns, Australia, he has garnered numerous accolades for his outstanding contributions to teaching and student learning.
In 2021, he received the JCU Dean's Learning & Teaching Award, and in 2022, he was honored with the James Cook University Citation for Outstanding Contribution to Student Learning Award. He is currently doing a PhD at James Cook University, Australia.
With over 17 years of teaching and research experience in dental radiology, Dr. Sholapurkar has published extensively. He has authored over 50 articles in peer-reviewed dental journals, contributed 11 book chapters, and edited "Publish and Flourish — Practical Guide for Effective Scientific Writing." He has delivered guest lectures and keynote addresses at dental conventions, specialty conferences, and continuing professional development activities in Australia and abroad.
Additionally, he is involved in running Cone-beam Computed Tomography (CBCT) licensing courses and OPG/Lat Ceph licensing courses across Australia, contributing to the professional development of dental practitioners. He also regularly runs CBCT and 2D Radiology interpretation courses.
Dr. Amar Sholapurkar's courses has been verified by the New Zealand Dental Association and can be seen on their website.