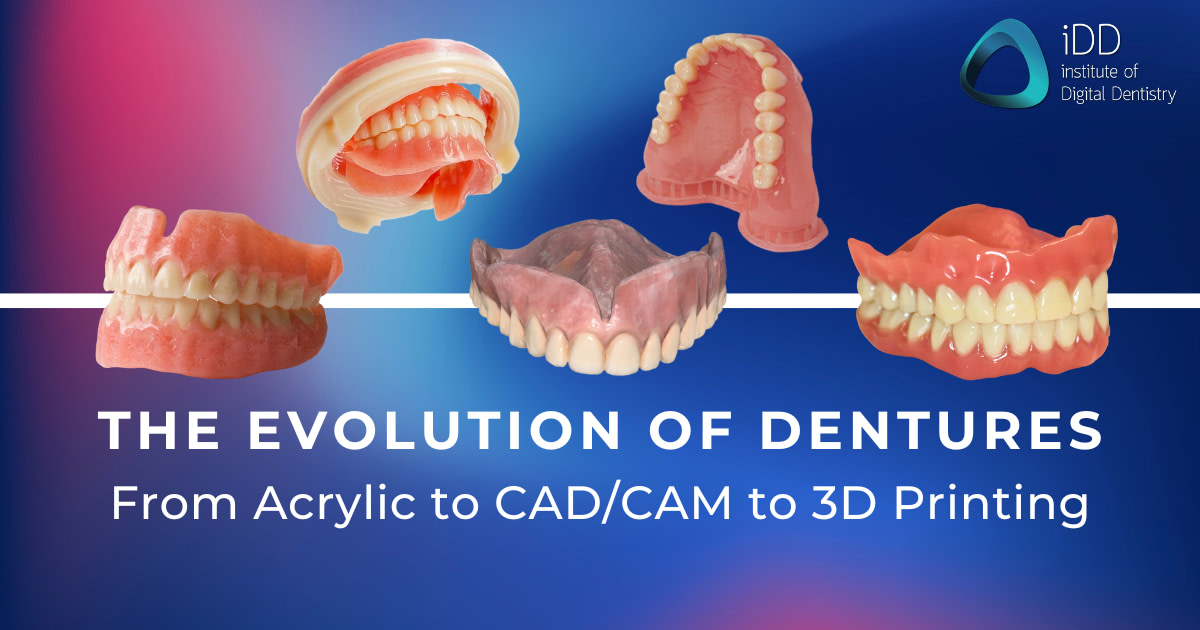
Dentures, a longstanding solution for tooth loss or edentulism, have been integral to dental care for generations.
Traditionally crafted from acrylic, these dental prostheses have been a mixed blessing. While they restore basic oral functions and aesthetics, traditional dentures have notable challenges. The fitting process is often intricate and time-consuming, demanding multiple dental visits and adjustments.
Comfort is another significant concern, as these dentures can cause soreness or irritation, compromising quality of life. But, the aesthetic aspect, though better than toothlessness, sometimes needs a natural appearance. It's a reality many have reluctantly accepted, faced with the daunting prospect of navigating social situations with a less-than-perfect smile. This can lead to psychological discomfort, with individuals feeling self-conscious about their smiles, impacting their social interactions and personal confidence.
Like the transition from landlines to smartphones, dentures have undergone a remarkable transformation. They've shifted from the traditional acrylic models once a staple in dental practices worldwide, echoing the broader shifts in technology and materials science.
Traditional Acrylic Dentures
Using acrylic in denture fabrication marked a significant advancement in dental prosthetics. Acrylic dentures became popular due to their relative ease of production and affordability, making them accessible to a broader population.

Polymethyl methylacrylate (PMMA) being poured into flask for traditional flasking/packing of a heat-cure denture. Image source.
They offered a semblance of natural teeth and gums, improving the aesthetic outcomes for patients. However, the limitations of acrylic dentures soon became apparent.
While initially fitting well, the material tends to deteriorate over time, leading to fit issues that require readjustment or complete replacement. This wear and tear could lead to discomfort, with patients often experiencing sore spots or difficulty chewing.
Furthermore, acrylic dentures required rigorous maintenance, as they were prone to staining and retaining odors, necessitating meticulous cleaning routines.
Transitioning from Traditional to Digital Dentures
While traditional acrylic dentures have served as a staple prosthodontic treatment for decades, the future of denture materials leans towards newer biocompatible resins, promising a new era of dentistry that prioritizes both health and aesthetic outcomes.
The advent of digital dentistry has been a game-changer in prosthodontics. Incorporating advanced technologies like 3D printing and Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM) has revolutionized how dentures are designed and fabricated. This digital revolution has allowed for the precise customization of dentures, tailoring them to the unique contours of each patient’s oral cavity.
With the rapid advancement of digital dentistry, this revolution of CAD/CAM technologies to mill dentures and 3D printing dentures completely transformed the denture fabrication process.
The result?
Custom-made, precise, and comfortable dentures.
Furthermore, the introduction of new materials, in conjunction with dental technologies, has led to the production of dentures that are more durable, more comfortable to wear, and more closely mimic the appearance of natural teeth.
This progression from traditional to digital dentures offers a promising solution to a long-standing problem, paving the way for a future where dentures promise comfort, convenience, and confidence.
CAD/CAM Milled Dentures
CAD/CAM milling removes the denture from a solid block of the chosen material, ensuring uniformity and a bespoke fit.
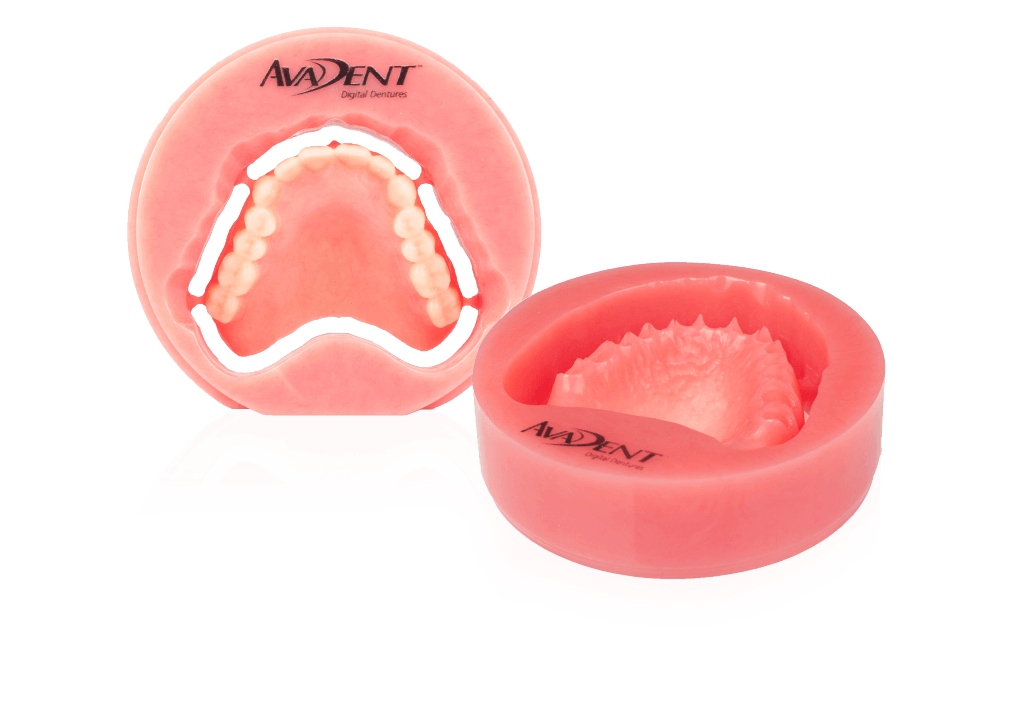
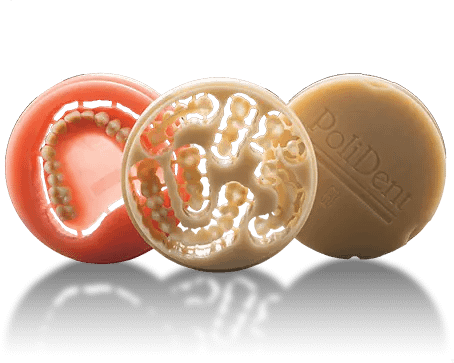
Nowadays, CAD/CAM milling for complete denture fabrication has become commercially available with the introduction of AvaDent digital dentures, the Polident CAD/CAM dentures, and Ivotion by Ivoclar.
According to a clinical report by Dr Nadica Janeva, full/full (F/F) digital dentures were fabricated from pre-polymerized AvaDent resin acrylic pucks with SR Vivodent DCL teeth bonded in the milled tooth sockets. The digital denture-making process offers various advantages compared to conventional heat-cured, flasking, and packing acrylic dentures. This included fewer visits, less clinical chair time, and the ability to quickly produce spare or replacement dentures from stored digital data in the manufacturer's database.
Furthermore, milled dentures, crafted from prepolymerized acrylic resin pucks created through a high-pressure, high-heat process, did not experience polymerization shrinkage, which reduces porosity and lowers the adherence of Candida albicans to the denture base.
Consequently, milled dentures provided a more precise fit and improved retention due to their absence of polymerization shrinkage compared to conventional dentures. Keep in mind that additional research is necessary as the available information on milled dentures is currently limited and mainly consists of case reports and proof-of-concept studies.
3D Printed Dentures
On the other hand, 3D printing is a marvel in its own right. 3D printing has the capability of constructing dentures layer by layer. This ensures an exacting precision that is hard to achieve consistently through traditional methods.
Enter biocompatible resins, a revolutionary material turning the tables in the denture world. This advanced material has enhanced strength and durability, ensuring the dentures last longer and perform better.
The main advantage lies in their biocompatibility.
These resins are designed to work in harmony with the biological systems of the human body. This means a reduced risk of allergic reactions and better overall comfort for the patient.
Furthermore, they offer superior aesthetics with their translucent properties, closely resembling the natural appearance of teeth and gums.
Here are some examples of current denture resins available on the market today:
Dentca Denture Resin
Dentca Denture Resin from Whip Mix is the first 3D-printed resin to receive FDA clearance. Their physical properties and biocompatibility pass FDA requirements and give printed denture properties similar to conventional ones. The Dentca 3D printable resins include an ivory-colored try-in material, tooth materials in Vita shades A1, A2, A3, A3.5, B1 & B2, and denture base materials in Original Pink, Light Pink, Reddish Pink & Dark Pink shades. It’s worth noting that Dentca Denture Resin is available for sale in the US only at this point.Flexcera Dental Resin
The Flexcera Dental Resin range from Desktop Health includes the dental base resin material, Flexcera Base, and accompanying acrylic teeth resin material, Flexcera Smile, and Flexcera Smile Ultra+. Flexcera Smile Ultra+ is an FDA 510(k) Class II cleared, MDR Class IIa certified, and CE-marked medical device for the additive manufacturing of permanent or temporary artificial teeth for dentures, crowns, bridges, inlays, onlays & veneers, and complete, monolithic, or partial dentures.Formlabs Denture Resin
Formlabs Denture Resins are certified biocompatible materials for 3D printing digital dentures. From Light Pink (LP), Original Pink (OP), Red Pink (RP), and Dark Pink (DP), these four semi-translucent shades allow for a more custom 3D printed denture where clinicians and technicians can achieve lifelike gingiva with natural marginsGraphy Resin TFDH Denture Base
Graphy Resin TFDH Denture Base is the world's first 3D printable biocompatible flexible denture material. It can be used with both DLP and LCD printers. Chelsea Homire CDA, has previously reviewed the Graphy Tera Herz Flexible Base.Kulzer’s dima Print Digital Denture
Kulzer’s dima Print Digital Denture solution consists of three class IIa materials: dima Print Denture Base Try-in for the production of Try-ins, as well as dima Print Denture Teeth and dima Print Denture Base for the production of high-quality duplicate dentures with multiple shade options.Lucitone Denture Resin
Lucitone Denture Resin from Dentsply Sirona is a widely recognized material used in the fabrication of dentures and is one that iDD deems to be the best resin available on the market . This high-quality resin is known for its exceptional strength and durability, making it a preferred choice for both dental professionals and patients. Lucitone resins are designed to resist wear, fracture, and discoloration, ensuring long-lasting performance and aesthetic appeal.
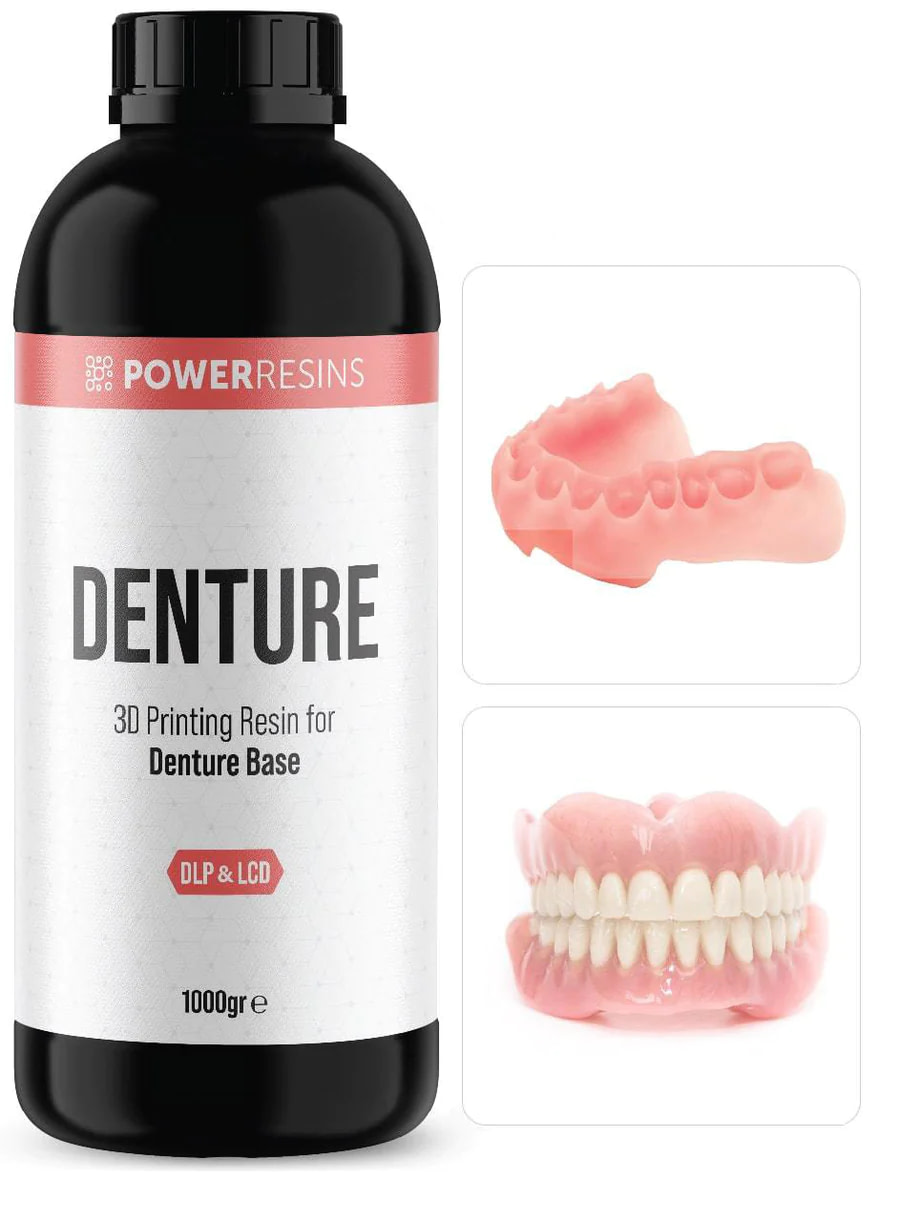
Powerresins Denture Base
Powerresins Denture 3D Printing Resin for Denture Base from DentaFab is another available resin material.Rodin Denture Base
Rodin Denture Base by Rodin is another material option for 3D printing dentures. As a biocompatible Class II material suitable for printing all types of denture bases, its high strength and low shrinkage properties produce excellent fitting denture bases.
SprintRay High Impact Denture Solution
SprintRay has a line of 3D printer resin for the denture base and teeth. SprintRay High Impact Denture Solution is the company’s workflow solution to streamline the treatment process for patients. It is designed to decrease the time spent in the chair and deliver removable dentures in as few as 2 appointments. SprintRay also manufactures a Try-In 3D printer resin material to get the fit right before utilizing their definitive, 2-piece High Impact denture.
It's important to know that all 3D printing resin liquid materials, including denture (base) resins, should be stored in a dark and moisture-free place at room temperature (20-24 °C). Also, remember to shake or mix the resin well before use to ensure optimal print quality.
Limitations with Digital Dentures
CAD/CAM dentures have been associated with several clinical disadvantages, including material wastage, high costs, immediate reline, occlusal vertical dimension (OVD) issues, and compromised aesthetics and phonetics.
Furthermore, some researchers have noted additional complications with CAD/CAM dentures, such as errors in occlusion and tooth arrangement, tooth wear, increased follow-up visits, post-insertion adjustments, overall patient dissatisfaction, and the need for remakes.
In contrast, 3D printed dentures share some clinical disadvantages with CAD/CAM dentures, including material wastage, high costs, and compromised aesthetics. Still, they also present unique challenges, such as reduced retention and lower strength.
Compared to traditional denture manufacturing methods, these drawbacks are generally considered the primary limitations and hurdles for CAD/CAM and 3D-printed dentures.
An interesting comparison between CAD/CAM and 3D printed dentures was made in another case study by Dr. Corina Cristache, who highlighted that CAD/CAM dentures tended to be more expensive and resulted in more significant material wastage, whereas 3D printed dentures were more cost-effective and offered the ability to produce intricate details with high precision.
These findings underscored the significance of material conservation, a key advantage of 3D printing technology over CAD/CAM manufacturing methods, contributing to the affordability of 3D printing systems compared to CAD/CAM systems.
For those interested in reading more about the clinical use of CAD/CAM and 3D printed dentures, I recommend reading this article by Dr Khaled Allahak for an in-depth review of the advantages and disadvantages of the digital denture workflow and treatment outcomes.
Conclusion
The ultimate aim remains to provide patients with dentures that restore functionality and offer unparalleled comfort and aesthetics.
The transition from traditional acrylic to biocompatible resins signifies a significant advancement in prosthodontics. These modern materials are set to bridge the gap between functionality and aesthetics, paving the way for the future of denture materials.
So, from traditional acrylic to modern biocompatible resins, the future of technology and denture materials continues to evolve. Commercially accessible CAD/CAM denture systems are anticipated to address the drawbacks commonly associated with traditional manufacturing methods.
Dentistry will continue to seek ways to improve upon these materials, pushing the boundaries of what is possible.
Let us know in the comments below how you manufacture your dentures! Do you prefer sticking to the traditional flasking/packing or are you implementing digital dentistry and milling or 3D printing your dentures in your practice or lab?
Discover more on digital dentures with iDD. We have several courses for further education if you want to expand your denture knowledge.
Learn the digital denture clinical workflow from world-renowned denturist Dr. Eric D. Kukucka in iDD's online course, Digital Dentures. His digital workflow and how he captures the patient's edentulous arches, their relationship (bite), and soft tissues to achieve a denture that is aesthetic, highly functional, comfortable, and reliable.

Alternatively, learn how digital dentures can be done simply and economically with Dr. August de Oliveira in his comprehensive online course with iDD, 3D Printed Dentures - Efficient Workflows for Dentists. In this course, he covers the intricacies of digital dentures, from scanning edentulous patients to 3D printing and post-processing.










I decided to have digital dentures as the dentist told me that I would have a better fit, but I have had more trouble with my bottom set compared to ordinary dentures.The cost just isn’t worth it.
Hi there. The fit of digital dentures can vary and often depends on several key factors including the accuracy of the scan, the quality of the design, and the precision of the manufacturing process. When done well, they can offer excellent fit and reproducibility, but as with any dental treatment, results can vary between cases.
We’d strongly encourage you to speak with your treating dentist about the concerns you’re having. They’ll be in the best position to assess the fit and make any necessary adjustments or discuss other options to improve your comfort.
Wishing you the best on your dental journey.