I've just wrapped up work on a comprehensive white paper with Avant Dental (a large Lab in Australia) that addresses a crucial issue - why some All-on-X cases deliver life-changing results while others fail spectacularly, despite seemingly identical surgical execution.
While working on this white paper we identified four phases of treatment where most complications originate.
What became clear through this collaboration is that success with full-arch implants has surprisingly little to do with surgical heroics and almost everything to do with systematic planning, realistic patient selection, and honest expectation-setting.
Here's what you need to know if you're offering All-on-X, or considering adding it to your practice.

The Reality Check - Digital Tools Aren't Magic
Let me begin with something that needs to be said.
Digital dentistry has genuinely transformed full-arch workflows. We can now scan, design, and deliver in timeframes that would've seemed impossible a decade ago.
Photogrammetry-enabled scanners, IPG, in-practice 3D printing, and streamlined CAD workflow technologies offer real advantages.
But here's the catch: these tools only work if you understand their limitations and use them properly.
As I noted in the white paper, "Digital dentistry is not just about new tools. It's about new ways of thinking. The challenge is not whether we scan or print; It's whether our workflow is integrated, efficient, and predictable."
The question becomes: Are practices investing in digital systems actually taking time to master them, or are they hoping the technology will compensate for gaps in planning and execution?
What we're seeing in the field suggests that equipment ownership doesn't necessarily equate to competency. And in All-on-X cases, that gap between ownership and mastery shows up quickly.
Step 1: Patient Selection – Where Most Cases Fail Before They Start
One of the biggest predictors of All-on-X failure we identified isn't surgical technique. It's patient selection.
Dr. Gupta puts it perfectly in the paper: "You need a clear line between what's a red flag and what can be managed with planning. If you miss that, the case will go wrong – fast."
What Actually Matters in Patient Selection
The white paper breaks down patient eligibility into several critical categories:
Medical and anatomical factors are straightforward - bone volume, systemic health, and healing capacity. These are the criteria most practices already evaluate.
But here's where it gets interesting: behavioral and psychological factors are equally important, yet they're often dismissed or minimized during case acceptance.
Consider these scenarios:
- A patient with a history of poor hygiene who lost their teeth to neglect
- Someone who consistently missed dental recall appointments
- A patient with unrealistic aesthetic expectations who refused to compromise during planning
- Anyone unwilling to commit to structured maintenance protocols
The white paper is blunt about this: patients who have historically demonstrated poor compliance are unlikely to maintain a full-arch prosthesis successfully.
As Dr. Gupta warns: "We see so many patients who lost their teeth to neglect, and they assume implants won't need looking after. That mindset will destroy a full-arch case."
The Structural Planning Nobody Talks About
There's another layer that deserves more attention: structural constraints that determine whether a case is even mechanically viable.
The paper emphasizes critical factors like:
- A-P spread (anterior-posterior spread), determining how far the prosthesis can safely extend
- Restorative space accommodating the full prosthetic stack without compromising strength
- Hygiene access, ensuring patients can actually clean around the prosthesis
- Cantilever length staying within safe limits relative to A-P spread
Dr. White's perspective is valuable here: "A-P spread and restorative space need to be understood from day one. If you don't account for cantilever forces, hygiene access, and bone reduction at the start, you're compromising the final outcome."

The Business Reality We Need to Acknowledge
Here's where I think many practices get into trouble. There's financial pressure to accept marginal cases - patients who might be anatomically suitable but behaviorally high-risk.
The white paper includes an excellent table of red flags covering medical, behavioral, anatomical, functional, and psychological exclusion criteria. But the real question is: how many practices actually turn patients away based on these criteria?
When you've invested significantly in All-on-X training and equipment, saying "no" to paying patients becomes harder. That's a reality we need to acknowledge. The most successful practices will be those with the discipline to decline unsuitable cases, even when it hurts the bottom line in the short term.
Step 2: Digital Workflow – Precision With a Steep Learning Curve
The scanning and digital workflow section highlights something we discuss regularly here at iDD: accuracy is everything in full-arch cases, and even minor errors compound quickly.


The Intraoral Photogrammetry Promise
Systems like the Shining 3D Aoralscan Elite, which integrate ‘photogrammetry”, can capture implant positions with remarkable precision. This technology has genuine potential to improve outcomes and reduce the number of appointments.
However, Dr. White shares their real-world experience: "We've trialled photogrammetry in-house and with labs. The precision is great, but if the lab doesn't have the software or you get the scan body placement wrong, it's a nightmare to fix."
This is exactly the kind of assessment we need more of in digital dentistry. The technology works, but it requires:
- Proper training on software and workflows
- Lab partnerships with compatible software systems
- Systematic protocols for quality control
- Understanding when things are going wrong and how to fix them
Streamlined Workflows: Reality vs. Marketing
The white paper acknowledges that digital workflows can reduce full-arch cases from five visits to two, or even same-day delivery in ideal situations. That's impressive and genuinely valuable for appropriate patients.
But let's be clear about the prerequisites that make this possible:
- Complete system integration (scanner, software, manufacturing)
- Extensive team training on protocols if doing everything in-house
- Lab partnerships are often required for manufacturing with compatible systems and proven expertise
- Clinical discipline to prevent shortcutting verification steps
I need to emphasize something crucial that often gets lost in marketing: "Speed should never come at the expense of occlusion, phonetics, or hygiene access."
How many practices remember this when marketing "teeth in a day"? There's a real tension between the competitive pressure to offer rapid delivery and the need to maintain high standards.
The Lab Communication Challenge
One issue that deserves more attention: miscommunication between clinic and lab around scan bodies, file types, or design expectations often causes delays or complete misfits.
The white paper recommends:
- Confirming scanner-software-lab compatibility before scanning
- Using validated scan body libraries for each implant system
- Sharing clear instructions with supporting photos, not just STL files
- Setting review points for the provisional design before finalization
These may sound like basic steps, but in practice, many workflow failures can be traced back to assumptions about compatibility or inadequate communication protocols.
Step 3: Materials – Beyond the Marketing Claims
Material section ranging from PMMA to monolithic zirconia to printed solutions. Each material has real advantages, but also limitations that you and patients need to understand upfront.
Dr. Gupta's perspective resonates: "Patients think once it's in, it's done. But the material you use, and how you get there, shapes everything – how it looks, how it lasts, how it feels to live with."
The Material Trade-offs Nobody Explains Properly
The white paper includes a helpful comparison table, but let me highlight some key points:
PMMA: Cost-effective and easily adjustable, but more prone to wear and fracture. It's excellent for temporaries and cost-sensitive cases, but patients need to understand it may require repair or replacement within 3-5 years.
Monolithic zirconia: High strength and excellent polishability for hygiene, but can be unforgiving to opposing dentition. Great to use for bruxers and high-durability cases, but requires careful occlusal management.
Hybrid solutions (titanium-acrylic): Moderate strength with good aesthetics, offering a middle ground between PMMA and zirconia. The challenge is ensuring proper interface management between components.
And of course, we have the printed solutions becoming popular on the market like Sprintray Onyx Tough and PacDent Titan. These are best treated like PMMA, but are much easier to manufacture than milling PMMA and have great applications in chairside CAD/CAM.

The Sustainability Question
Here's something worth considering: are practices being upfront about the likelihood of repairs or replacements when patients choose "economical" options, or with all on x in general?
When a patient selects PMMA to reduce initial costs, do they truly understand the long-term cost implications? The white paper addresses this, but it's an area where I believe our profession needs more open and honest conversations with patients.
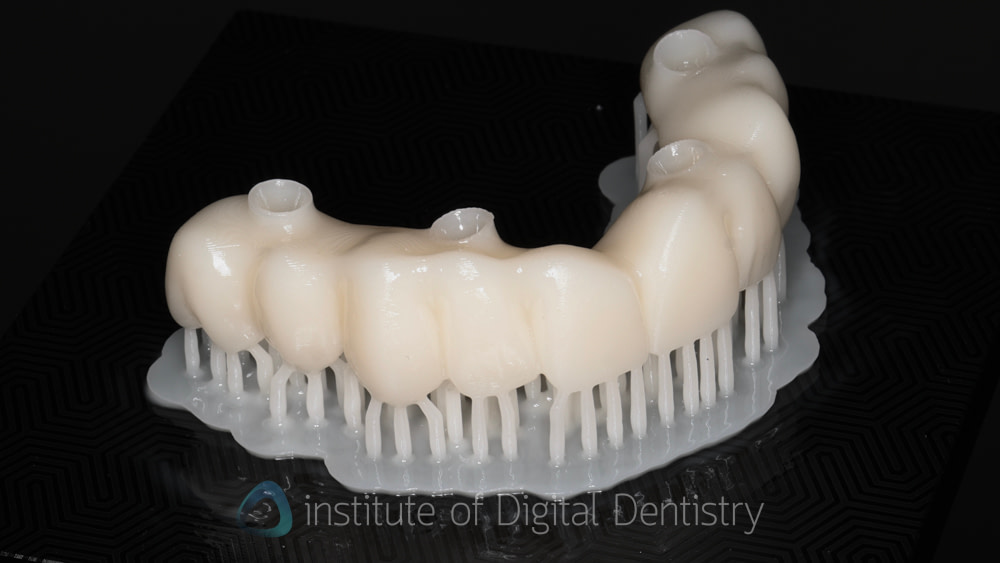
3D Printing: Promise and Reality
In-practice 3D printing for temporaries holds genuine promise for reducing wait times and costs. The white paper acknowledges the potential while highlighting the challenges.
Dr. White's warning is important: "We're printing same-day temps chairside now. But you've got to know your system. You can't just hit 'print' and hope. It needs calibration, polish, correct finishing, and post-processing protocols."
The key requirements for success:
- Validated material compatibility for intraoral use and all-on-x indications
- Proper printer calibration and software settings
- Systematic post-processing protocols
- Quality control checks before delivery
This is where I worry about practices that invest in printers without investing proportionally in training and quality control systems. The hardware is the easy part, it's the workflow integration that determines success.

Step 4: Maintenance – The Forgotten Phase That Determines Long-term Success
Post-treatment maintenance is absolutely critical for long-term success, yet it's often neglected in full-arch implant treatment.
Debunking the "Fit-and-Forget" Myth
Dr. White nails it: "Patients sometimes think once they have implants, they're set for life. But maintenance is essential for the durability and health of implants long-term". There is also an important discussion with the patient that needs to be had: ‘Nothing lasts forever, not even implants,’ and all on x.
Regarding maintenance protocols for full arch implant treatment, here is an example:
- Immediate follow-up (1-2 weeks): Healing confirmation and hygiene reinforcement
- Mid-term review (3-6 months): Radiographic checks and early complication detection
- Annual assessments: Long-term integrity monitoring
How often are you removing the prosthetic to clean underneath? And here's the critical question: how many practices actually enforce these protocols, rather than just hoping patients return voluntarily?
The Hygiene Reality Check
Without diligent daily cleaning and professional maintenance, patients risk accelerated bone loss and implant deterioration.
Some key hygiene instructions for patients may include:
- Water flossing beneath the prosthesis
- Brushing twice daily with appropriate techniques
- Antibacterial rinses as recommended
- Biannual professional cleanings with removal of the prosthetic
However, providing instructions isn't the same as ensuring compliance. Successful practices need systems for:
- Demonstrating correct hygiene techniques repeatedly
- Tracking patient compliance through recall programs
- Identifying early warning signs of neglect
- Having difficult conversations when patients aren't maintaining properly
Early Complication Detection
A crucial aspect to consider is that early identification and prompt intervention for peri-implantitis inflammation can significantly impact long-term outcomes.
This requires educating patients about warning signs:
- Gum inflammation or bleeding
- Persistent discomfort
- Prosthetic instability or movement
- Changes in bite or occlusion
However, it also requires practices to have rapid-response protocols in place when complications are suspected, rather than waiting for the next scheduled appointment.

The Ethical Dimension Nobody Wants to Discuss
Another critical aspect to consider is the ethical implications of funding. This is uncomfortable territory, but it's important.
All-on-X treatments represent a significant investment, and patients may not fully grasp the long-term financial commitment.
Here's what we need to acknowledge: practices have a financial incentive to proceed with cases, while patients may be making emotional decisions about replacing failed dentition. How do we ensure truly informed consent in this environment?
Some basic recommendations include:
- Transparent documentation of financial implications
- Clear disclosure of ongoing maintenance costs
- Honest discussions about the total cost of ownership over 10-20 years
The question is whether they're actually being implemented consistently across practices offering All-on-X. Should there be standardized disclosure documents for full-arch cases? How do we balance making treatment accessible while ensuring patients can actually afford long-term maintenance? These questions don't have easy answers, but we need to be asking them.
The Bottom Line
All-on-X can deliver life-changing outcomes for appropriate patients when executed properly. But "properly" means:
Rigorous patient selection - and the courage to say no to unsuitable casesMastery of digital workflows - not just ownership of equipmentRealistic material selection - aligned with patient expectations and budgets Structured long-term maintenance - actually enforced, not just recommended
As more practices adopt full-arch workflows, we can expect to see an increasing variation in outcomes. The practices that succeed will be those that resist the temptation to oversimplify or overpromise, and instead invest in systematic approaches to every phase of treatment.
The digital tools we have access to are incredibly powerful. Photogrammetry and horizontal scan bodies can capture implant positions with precision that was previously impossible. With in-practice 3D printing, we can deliver temporaries on the same day. Streamlined workflows can significantly reduce the number of patient visits.
But these technologies aren't a substitute for clinical judgment, thorough planning, honest patient communication, and rigorous follow-up protocols. They're enablers that work best when integrated into well-designed systems operated by properly trained teams.
Your Thoughts?
If you're offering All-on-X in your practice:
- How do you handle patient selection for marginal cases - what are your absolute exclusion criteria?
- What's your experience with digital workflows - has reality lived up to the promise?
- How do you ensure patients actually comply with long-term maintenance protocols?
- What material choices have you found most successful for different patient profiles?
And if you're considering adding All-on-X to your services, this white paper is worth reading in full. The detail in the red flags table, workflow stages, and material comparisons alone makes it valuable reference material.
The comprehensive tables and detailed protocols offer practical guidance that extends beyond what can be covered in a blog post.
You can access the complete white paper by clicking the button below.
What's been your experience with full-arch implant cases? Are there any lessons you'd like to share with the iDD community? Drop your thoughts in the comments below.
Full disclosure: I contributed to this white paper alongside Dr. Hitesh Gupta and Dr. Cameron White, with content authored by Ian Feigen from Avant Dental. While I'm enthusiastic about the potential of All-on-X treatments when done properly, I believe our responsibility is to provide balanced analysis that helps practices succeed sustainably, and that means acknowledging challenges and limitations as honestly as we celebrate opportunities and innovations.